Article Info
Nasr Tantawi
Year: 1993
Month: September
Issue: 1
Pages:
Reference:
Al-Gahtani Y., Al-Gahtani M.,Nasr Tantawi .Saudi Epidemiology Bulletin. 1993;1(1):.
On July 20 and 21, 1992, 167 Indian workers at an agricultural company developed diarrhea. The company grows and processes vegetables, fruits and grain on 35,000 hectares of land 50 kilometers north of Tabuk city. It employs 1,100 workers of seven different nationalities: Indian, Turkish, Egyptian, Saudi, Thai, Filipino and American. All workers live in barracks or tents. There is one bathroom for every 10 workers.
Food is prepared and supervised by another company, and each nationality has its own chef and assistants. Food poisoning occurred in this camp in 1990 among Filipino workers and in 1992 among Egyptian workers.
We interviewed all Indian laborers to determine which of the 17 food items served on July 19 they had eaten, the exact time their symptoms had begun and the type of symptoms they had reported. We defined a case as any person who ate the Indian meal on July 19, 1992, from 5 p.m. to 9 p.m. and who developed abdominal cramps and/or diarrhea within the following 48 hours. We asked the kitchen workers how they prepared the food.
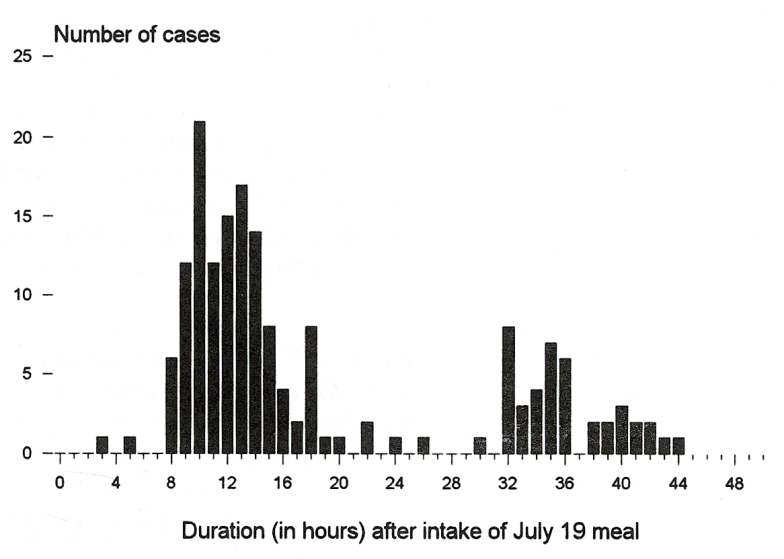
Of 221 workers who ate the Indian food on July 19, 1992, 167 (79%) fit our case definition. No case had fever and 2 percent reported vomiting. Diarrhea and other symptoms resolved within 12 hours of onset. There were two peaks in the epidemic curve: the first 12 hours after the workers finished the supper July 19 and the second 12 hours after they finished supper July 20 (chart). Kitchen workers who prepared food but did not eat it did not develop diarrhea.
Workers who ate yogurt had an attack rate (cases per 100 exposed) of 99%, compared with 12% for workers who did not eat yogurt (risk ratio = 9.6; 95% confidence interval = 4.5-20.4).
No other food eaten on July 19 was associated with illness.
Preparation of yogurt begins at 9 p.m. Dried milk in 50-kilogram plastic sacks is mixed in 82-liter cooking pots with water, leftover yogurt and three tins of concentrated yogurt. The mixture is left at room temperature (40 degrees centigrade) in a non-functioning cold room until 5 p.m. the next day. Clostridium perfringens was isolated from yogurt collected on July 20 and from the food table where the yogurt is prepared.
Editorial note:
Since Hobbs in 1953 showed that Clostridium perfringens caused foodborne disease, this organism ranks with Salmonella and Staphylococcus as one of the three most common causes of foodborne outbreaks of gastroenteritis. It exists widely in the environment and persists for years as spores. It is a normal inhabitant of the gastrointestinal tract of humans and other mammals, but it does not produce diarrhea unless ingested in large amounts (108 organisms per gram of food). The diarrhea is produced by preformed toxins elaborated while the organism is multiplying rapidly in the food.
C. perfringens food poisoning is recognized on epidemiologic and clinical criteria. It always occurs as outbreaks in persons sharing a common food. Patients present with diarrhea and abdominal cramps without fever. Nausea can be present but vomiting is rare. The diarrhea begins 12 hours (range 8 to 16) after eating the contaminated food and lasts about 12 hours (range 6 to 24). These features are clearly distinct from staphylococcal food poisoning and salmonellosis. The diagnosis is confirmed by demonstrating >= 10 C. perfringens per gram of food. If anaerobic culture facilities are not available, a direct smear of the food will show square-ended, gram-positive bacilli almost exclusively.
In this outbreak yogurt was implicated both epidemiologically and microbiologically. To produce C. perfringens food poisoning, one needs to subject the food to anaerobic conditions and temperatures between 20 and 50 degrees centigrade for several hours. The yogurt was kept at 40 degrees centigrade for 21 hours in large containers (i.e. anaerobic conditions); thus all three conditions were ideal. This outbreak presented with a biphasic epidemic curve probably because the yogurt was contaminated on both July 19 and July 20 (proven by culture); leftover yogurt from July 19 used as starter was the contaminant on July 20.
C. perfringens is most commonly found in meats and stews prepared in large amounts. Because spores survive cooking, food cooked in large volumes must be eaten immediately after cooking or cooled rapidly to 4 degrees centigrade. Since C. perfringens is widespread on meats, on poultry and in the environment, microbiological testing of the kitchen environment or of food handlers has little value in the prevention or investigation of C. perfringens food poisoning. Prevention rests on strict attention to correct storage time and temperature of foods cooked in large volumes.