Article Info
Year: 2006
Month: July
Issue: 3
Pages:
Reference:
Hyani O., Al-Rabeah A., Alhamdan N., .Saudi Epidemiology Bulletin. 2006;13(3):.
An increase in the number of Hepatitis A cases was reported from scattered villages in DhulaiE¼a Rasheed, Qassiem region. A case control study was conducted to describe this outbreak, identify possible risk factors and provide recommendations for control and prevention. A case was defined as any person living in DhulaiE¼a Rasheed governorate and presenting at one of the health facilities with jaundice and/or diagnosed as suffering from hepatitis A clinically and/or confirmed by laboratory tests during the period of 14/9/1426 to 1/4/1427 (18 October 2005 to 30 April 2006). Two controls were selected for each case. Data was collected by face to face interviews.
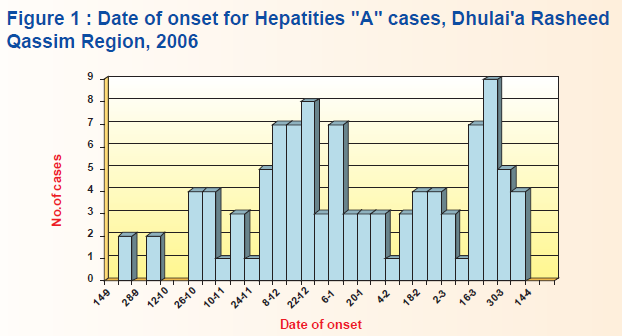
The outbreak occurred in the period between 11/08/1426 to 01/04/1427 H. The epidemic curve showed five peaks which most likely represented a person to person spread and maybe some sort of extended common source (Figure 1).
The cases were scattered in 20 different villages, with varied distances. Their ages ranged from 3-12 years (mean ±SD = 5.4±2.2). There were 62 males (59.0%), and 43 females (41.0%). Nineteen were students attending different primary schools. All were Saudis. We were able to interview 210 controls who fulfilled the criteria of the control definition. Their ages ranged from 3-13 years (mean ±SD = 6.2 ±2.3), there were 119 males (56.7%), and 91 females (43.3%), and 61 were students at primary schools, all were Saudis.
Significant Risk factors identified were contact with a known case (OR=1.7, 95% CI=1.01-2.95). The risk was much higher when the cases were relatives (OR=7.79, 95% CI= 1.10 €“ 67.13). Contact with a neighbor with jaundice (OR=4.44, 95% CI=2.15-9.23) was also statistically significant.
The study showed that 74.3% of cases washed their hands before eating, compared to 97.1% of controls (OR=0.09, 95% CI= 0.03€“0.21). Washing hands with water and soap before eating was reported by 5.1% of cases compared to 6.9% of controls (OR=0.06, 95% CI= 0.01 €“ 031). Washing hands after eating was reported by 76.2% of cases, compared to 98.1% of controls (OR= 0.06, 95% CI= 0.02-0.18). Also, 73.3% of cases washed hands after going to toilet compared to 95.2% of controls (OR= 0.14, 95% CI= 0.06 €“ 0.29). Washing hands with water and soap after going to toilet was reported by 11.7% of cases, compared to 10.5% of controls (OR=0.15, 95% CI= 0.05-0.50).
Immunization of the population at risk with Immunoglobulin (Ig) was carried out by the preventive department of Al Qassiem health directorate as part of the control measures applied. About 45.7% of controls had received the Ig, 30.5% of the cases had also been immunized, but they had received the Ig after acquiring the infection, therefore those who had received the Ig among the controls were protected against infection (OR= 0.52, 95% CI = 0.31-0.88).
There were 9 different water sources, represented by scattered shallow wells around DhulaiE¼a Rasheed area. The water was brought to the households by tank vehicles (Wayet) for all the 20 villages where the cases were reported. All the water samples which were taken from the nine wells and also the samples from different households and schools were chemically and biologically contaminated and incompatible for human use. The schools and shops in these areas used the same sources of water that was used by the houses. Indeed, there was no general sewage system in these villages; each house had its own sewage system, such as: Bayara or artesian-well-hole. These artesian-well-holes used for sewage disposal are done by digging a deep hole down to 40 meters below earth. We found that 98.1% of cases and 100% of controls used Bayara for sewage disposal, and 1.9% of cases and none of the controls used artesian well-hole, which meant that the type of sewage disposal was not a risk factor for acquiring the infection.
Editorial note:
Hepatitis is a common medical condition caused by a wide range of viruses: A, B, C, D & E.
Hepatitis A is one of the oldest illnesses in human record. It occurs sporadically and epidemically worldwide, with a tendency to cyclic recurrences.[1] It is endemic in many parts of the world, including Saudi Arabia, where viral hepatitis A is a major cause of morbidity. It has been observed that nearly 41% of cases of viral hepatitis in western Saudi Arabia were due to HAV.[1] Hepatitis A is considered endemic in most of the villages of Al Qassiem region. However, several factors could explain this local upsurge of the disease. In this study, shallow wells represented the only source of water supply to DhulaiE¼a Rasheed area, and are possible extended common source of infection, whether in household or school environments. Also, a person-to-person transmission pattern could be established due to a low socio-hygienic status. Unfortunately, facilities for HAV isolation with sub typing were not available and the outbreak was disrupted by passive immunization of most of the population.
It is well known that the best methods of control and prevention at endemic areas depend on eliminating the source of infection and identification of the mode of transmission. It was clear that transmission was in favor of person-to-person and one of the major risk factors was the neglect of the cases to follow basic hygienic practices by washing hands at least after going to toilet and before eating. Good personal hygienic practices play a significant role in protection against acquiring infection.[2]
This outbreak of Hepatitis A is very similar to previous outbreaks that occurred at rural communities in the Kingdom, in which person-to-person transmission was implicated.[4,5] This outbreak can also be treated as an exacerbation of the endemic person-to-person, feco-oral transmission of disease which is prevalent in such areas with poor water supply and low socioeconomic status. [2]
Immunoglobulin mass immunization applied by the preventive department of Al Qassiem health Directorate was efficient in controlling the outbreak when direct contacts were vaccinated. This was able to reduce the incidence of HAV secondary cases but could not stop new cases from appearing. Many studies consider passive immunization with immunoglobulin as the first choice in prevention and control of HAV epidemics and as a post exposure prophylaxis.[6] The effectiveness of the Ig lasts only for a few months, so it is required to be re-administered every three to six months.
The fact that scattered cases appeared in 20 villages within a period of 29 weeks may exclude the possibility of common source transmission. Drinking water from taps at houses or in the street was not associated with acquiring the disease, which proves that this was not a common source epidemic, which would have resulted in a much wider spread of cases and more family members would have been affected at the same time. However, the possibility of extended common source model could not be totally excluded, especially with the contamination of all water sources in the area and the significant association of drinking water from the school cooler with acquiring the infection. Underreporting may also play a role of underestimation of the strong endemicity of HAV in DhulaiE¼a Rasheed area.
References :
- Shobokshi OA, Serebour FE. The etiology of acute viral hepatitis in the western region of Saudi Arabia. Trans Soc Trop Hyg 1987; 81: 219-21.
- Ashraf SJ. Arya SC, Parande CM, et al. Hepatitis A virus among natives and expatriates in Saudi Arabia. J Med Virol 1986; 19:151-153.
- Ramia S. Antibody against hepatitis A in Saudi Arabians and in expatriates from various parts of the world working in Saudi Arabia. J Infect 1986:12:153-155
- Kholedi AN, Choudhry AJ, Turkistani AM. An outbreak of hepatitis A in Jizan, 2002. Saudi Epidem Bull; Vol 9(2).
- AlSaleh Essa, Turkistani AM, Nooh RM. Hepatitis A outbreak at Al-Berk, Asir region, 2004. Saudi Epidem Bull; Vol 12(1).
- Hollinger FB et al. Discussion: who should receive hepatitis A vaccine? A strategy for controlling hepatitis A in the United States. J Inf Dis, 1995; 171(Suppl 1): S73-S77.